Metabolic Program Patient Guide/Info
Checklist
- Initial consultation
- Completion of screening labs
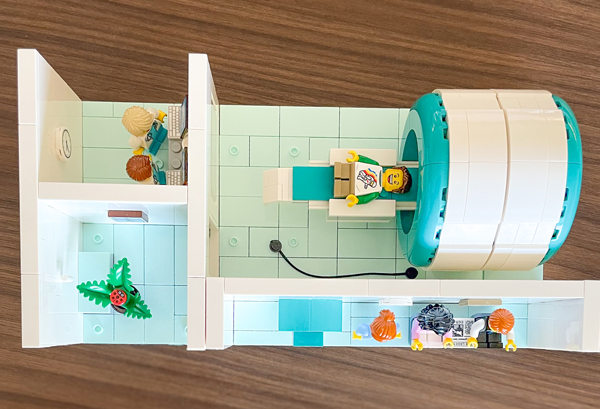
- Body composition scan
- Referrals to sleep medicine, nutrition services, and psychiatry for comprehensive evaluation and support
- Follow-up virtual pharmacotherapy visit (if GLP/GIP medication is prescribed)
- Follow-up medication and weight management visits (to help guide your progress)
Why are sleep, nutrition and psychiatry evaluations required as part of my treatment plan?
As part of your personalized weight and metabolic health program, we require assessments with sleep medicine, nutrition, physical therapy and psychiatric/behavioral health specialists. In addition to often being required by insurance companies to approve certain weight loss medications, these evaluations provide critical insights into your overall health and can help maximize your success.
Here’s why each one matters:
Sleep Health Evaluation
Poor sleep — including sleep apnea, insomnia, or irregular sleep patterns — can:
- Disrupt your metabolism and hormone balance
- Increase hunger and cravings (especially for carbs and sugar)
- Impair your energy levels and motivation to move
- Raise your risk for high blood pressure, insulin resistance, and other weight-related conditions
A sleep evaluation helps us uncover and treat issues like obstructive sleep apnea, which often go undiagnosed and can directly affect your ability to lose weight safely and effectively.
Nutrition Counseling
Even if you already have a good understanding of nutrition, meeting with a dietitian offers:
- A customized plan that fits your medical needs, preferences, and lifestyle
- Guidance around portioning, emotional eating, meal planning, and more
- Support for creating realistic, sustainable habits — no fad diets required
Nutrition is more than calories in/calories out — it's about fueling your body in a way that supports long-term health, satiety and metabolism.
Physical Therapy
Physical therapy (PT) is not just for people with injuries — it’s a proactive step to help support your long-term success. Here’s why:
- A physical therapist can help design a safe and effective exercise plan.
- PT helps prevent injury by identifying and addressing joint stiffness, muscle imbalances or movement patterns that could lead to strain or pain during activity.
- Learn techniques to reduce strain on joints like the knees, hips and back.
- With expert support, you’ll feel more confident and empowered to move safely and consistently.
Psychiatric/Behavioral Health Evaluation
Your emotional and mental health play a big role in your physical health. This evaluation helps:
- Screen for depression, anxiety, trauma, ADHD or disordered eating — all of which can impact weight.
- Offer strategies for coping, motivation and behavior change.
- Address any emotional ties to food, body image or self-worth.
This is a judgment-free, supportive step to ensure your brain and body are working together for success — and to connect you with tools and resources that can make the journey feel less overwhelming.
Can I be referred for a bariatric surgery consultation?
Yes — if you are interested, we can absolutely refer you to our Bariatric Program for surgical consultation.
Bariatric (or metabolic) surgery is one of several evidence-based options for weight management. It may be an appropriate choice if:
- BMI is ≥35
- BMI 30-34.9: Surgery should be considered for individuals with metabolic diseases such as type 2 diabetes, hypertension or sleep apnea. It may also be considered for those who do not achieve substantial weight loss through non-surgical methods (such as lifestyle changes or medications).
- You are ready to make long-term lifestyle changes and commit to follow-up care after surgery.
Even if you're not yet certain whether surgery is the right path for you, a consultation can help you explore your options, understand the risks and benefits and ask questions with a specialist team.
What is obesity?
Obesity is a chronic, complex medical condition where excess body fat can negatively affect your health. Obesity is influenced by many factors including genetics, hormones, metabolism, environment, behavior, social factors and more – much of which is out of your control.
Doctors typically diagnose obesity using Body Mass Index (BMI):
- A BMI of 30 or higher is classified as obese.
- A BMI of 25 to 29.9 is considered overweight.
But BMI is just one tool — it doesn't tell the whole story. We also consider where fat is stored, your muscle mass, and any related health conditions. During your evaluation with the Metabolic Clinic, you may have a body composition scan done to better understand where your weight (including fat and lean muscle mass) lies within your body.
Why It Matters
Obesity increases the risk of many chronic illnesses, including:
- Type 2 diabetes
- High blood pressure and heart disease
- Fatty liver disease
- Sleep apnea
- Certain cancers
- Joint problems and mobility issues
The Good News
Obesity is treatable — and even a modest amount of weight loss (5–10%) can lead to big health improvements. It’s not all about willpower — it’s about working with your body, not against it.
That’s why we approach obesity like any other medical condition — with science-backed tools, ongoing support and compassionate care tailored to your needs.
What is metabolic health?
Metabolic health refers to how efficiently your body regulates key biological processes — especially those related to energy, blood sugar, fat and hormone balance.
- Normal blood glucose levels (without insulin resistance or prediabetes)
- Healthy blood pressure
- Balanced cholesterol and triglycerides
- Low levels of inflammation
- Appropriate body fat distribution (particularly around the abdomen)
It’s possible to have obesity and still be metabolically healthy — and conversely, people with a “normal” weight may have poor metabolic health.
Poor metabolic health often goes unnoticed until symptoms or chronic conditions develop — such as type 2 diabetes, heart disease, fatty liver disease or PCOS.
Supporting Metabolic Health
Improving metabolic health doesn’t just mean losing weight. It includes:
- Eating in a way that keeps blood sugar steady.
- Moving your body to improve insulin sensitivity.
- Sleeping well to support hormone regulation.
- Managing stress to reduce inflammation.
- Using medications or other interventions when appropriate.
What are GLP-1 and GIP medications?
GLP-1 (glucagon-like peptide-1) and GIP (glucose-dependent insulinotropic polypeptide) medications are a class of treatments that help support weight loss and improve blood sugar control. They are designed to mimic natural hormones your body releases from the gut in response to eating.
These medications work by:
- Reducing appetite: They act on the brain’s appetite centers (especially the hypothalamus) to decrease hunger signals and increase feelings of fullness and satisfaction after meals.
- Slowing stomach emptying: This means food stays in the stomach longer, helping you feel full longer and reducing the desire to snack or overeat.
- Stabilizing blood sugar: These medications help the body respond more appropriately to food by increasing insulin secretion and reducing glucagon, a hormone that normally raises blood sugar. Together, these actions help prevent post-meal blood sugar spikes and promote more stable glucose levels throughout the day.
Newer medications that target both GLP-1 and GIP receptors (like tirzepatide) may provide greater effects on weight loss and blood sugar control, thanks to their dual action on different metabolic pathways.
Common Medication Names
- GLP-1 only: Semaglutide (Ozempic®, Wegovy®), Liraglutide (Victoza®, Saxenda®)
- GLP-1 + GIP: Tirzepatide (Mounjaro®, Zepbound®)
Additional Benefits
These medications may also help improve:
- Blood pressure
- Cholesterol
- Fatty liver (MASLD)
- Systemic inflammation
- Cardiovascular risk reduction (some are proven to lower risk of heart attack and stroke)
Important Notes
Most GLP-1 and GIP medications are injected weekly and may cause side effects such as nausea, constipation or fatigue — especially at the beginning. These often improve over time.
The injections are given with a very small, thin needle just under the skin and are typically painless or cause only minimal discomfort. Most patients find them easy to use and get comfortable with self-injection very quickly.
They are most effective when part of a full program that includes:
- Nutrition guidance
- Regular movement
- Behavior or mental health support
- Close medical monitoring
GLP-1 and GIP medications help recalibrate how the body regulates appetite and metabolism, making it easier to achieve and maintain a healthy weight and blood sugar — but lasting success still depends on a supportive lifestyle and follow-up care.
How much weight loss can I expect with GLP-1/GIP medications?
GLP-1 medications like semaglutide and tirzepatide have shown significant results in clinical trials and are currently the most effective weight loss medications on the market.
- Semaglutide: Patients typically lose around 15% of their body weight
- Tirzepatide: Average weight loss ranges from 15% to 20% of body weight, sometimes more
These results can vary based on individual factors like starting weight, adherence and lifestyle changes.
What if I don’t lose much weight on GLP-1/GIP medications?
While most people taking GLP-1 medications like semaglutide or tirzepatide experience significant weight loss—often 15–20% of their body weight—a small number of patients may not respond as strongly.
This is rare, but it does happen—and the reasons aren’t fully understood. It may be related to individual differences in biology, metabolism, gut hormone signaling, or how the body processes the medication. Other factors like medication adherence, lifestyle habits, or underlying health conditions can also play a role.
If weight loss is limited, we’ll work together to explore other options which may include medication adjustments, enhancing lifestyle support or consideration of bariatric surgery.
Are there other weight loss medications besides GLP-1/GIPs?
Yes—there are several other FDA-approved and off-label medications that may support weight loss, depending on your health history and goals:
Other Available Medications:
Qsymia (phentermine/topiramate ER):
A combination pill that reduces appetite and cravings. Supports weight loss of 5-10% of total body weight.
Contrave (naltrexone/bupropion):
Targets hunger and reward pathways in the brain. Can help with emotional eating, binge eating, and smoking cessation. Supports moderate weight loss of 4-6% of total body weight.
Orlistat (Alli, Xenical):
Blocks fat absorption in the gut. Works best when combined with a low-fat diet. Supports moderate weight loss of 4-6% of total body weight.
Metformin:
Originally used for type 2 diabetes, it’s also prescribed off-label for weight loss—especially in people with insulin resistance or PCOS. Weight loss is typically modest with expected loss of 2–5% of total body weight.
Will I need to be on long-term treatment for weight management?
That's an excellent question—and the short answer is yes, long-term treatment is often necessary. Obesity is a chronic, relapsing disease, which means it doesn’t have a cure, but it can be effectively managed over time. Just like conditions such as high blood pressure or diabetes, ongoing care is essential to maintain progress and prevent complications.
Here’s why long-term treatment matters:
Stopping treatment often leads to weight regain, which is why continued therapy—whether with medication, lifestyle support or both—is usually recommended. Many patients benefit from staying on anti-obesity medications long-term to maintain their progress.
Treating obesity often improves or even reverses other chronic conditions like type 2 diabetes, high blood pressure, sleep apnea and fatty liver disease. Continued treatment helps sustain these benefits and reduce long-term health risks.
We’ll work together to monitor your progress and adjust your treatment plan as needed. That might mean staying on the lowest effective dose, switching medications, or using intermittent therapy depending on your response and goals.
What diet is the best for weight loss?
The ‘best’ diet is one that you can stick to, enjoy and nourish your body with!
- Sustainability is key. The most effective diet is one you can maintain long-term—not just follow for a few weeks.
- Enjoyment matters. Choosing foods you genuinely like helps build lasting habits and reduces the feeling of restriction.
- Whole foods are foundational. Diets focused on minimally processed foods—like vegetables, fruits, lean proteins, whole grains and healthy fats—support better health and weight management.
- Limit processed foods, including refined sugars and carbohydrates. Reducing these can help stabilize blood sugar, curb cravings and support weight loss.
- Different approaches can work. Whether it’s low-carb, low-calorie or low-fat, the best plan is one that fits your lifestyle, preferences and health goals.
What are some helpful online tools for healthy eating and wellness?
Macronutrient and Calorie Tracking Apps
These apps help you log food, monitor macros and stay accountable:
- MyFitnessPal – Popular and widely used; offers a large food database and integration with fitness trackers
- Cronometer – Great for detailed nutrient tracking and those with specific dietary needs
- Lose It! – User-friendly app focused on calorie and macro tracking for weight loss
Healthy Eating & Meal Planning
These tools support balanced nutrition and meal prep:
- Eat This Much – Automated meal planner based on your calorie and macro goals.
- PlateJoy – Personalized meal plans with grocery lists and optional delivery integration.
- Yazio – Combines calorie tracking with meal planning and recipes.
Wellness and Lifestyle Support
Apps that support mindfulness, sleep and overall well-being:
- Noom – Behavior-based weight loss program with coaching and psychological tools.
- Headspace or Calm – For stress management, meditation and sleep support.
- Ate Food Diary – Visual food journaling to build mindful eating habits.
What are some cookbook recommendations?
The Doctor’s Kitchen by Dr. Rupy Aujla
Combines medical insight with flavorful, whole-food recipes.
Ideal for patients looking to improve overall health through diet
The Well Plated Cookbook by Erin Clarke
Focuses on fast, healthy recipes using accessible ingredients.
Each recipe includes options for dietary preferences .
Great for beginners and busy families.
Skinnytaste Meal Prep by Gina Homolka
Offers calorie-conscious, whole-food recipes with weekly meal prep plans.
Includes nutrition info and tips for portion control.
Very approachable for patients new to cooking or weight loss.
The Defined Dish: Healthy and Wholesome Weeknight Recipes by Alex Snodgrass
Focuses on clean, flavorful meals that are easy to prepare.
Includes gluten-free and dairy-optional recipes.
Popular among patients looking for practical, family-friendly meals.
Fit Men Cook by Kevin Curry
High-protein, whole-food recipes designed for weight loss and muscle maintenance.
Simple, budget-friendly ingredients with meal prep guidance.
Especially appealing to patients who want to stay active and eat well.
Healthy, My Way: Real Food, Real Flavor, Real Good by My Nguyen
Combines Vietnamese and California-inspired dishes with nutrient-dense ingredients.
Emphasizes flavor, texture and sustainable healthy eating.
Mostly Plants: 101 Delicious Flexitarian Recipes from the Pollan Family
Offers simple, flavorful recipes that emphasize plant-based ingredients with occasional meat and seafood.
Sustainable, whole-food eating that’s approachable for everyday home cooks.