Land AcknowledgmentWe acknowledge that the St. Charles campuses are located within the 10 million acres ceded to the Federal Government, also usual and accustomed areas, when the 1855 Treaty was signed with the Confederated Tribes of Warm Springs of Oregon. We offer this acknowledgment to honor all Native Americans that live in this area and who are the original people of this land. |
What is a land acknowledgment and why did St. Charles create one?
A land acknowledgment is a way for organizations and entities to recognize Indigenous people as the original stewards of the land upon which we reside and work. St. Charles is embracing this process in hopes that it can also serve as a tool for emotional healing that can help set a positive tone for future generations.
St. Charles recognizes that the health system and hospitals occupy land originally inhabited by Indigenous people, who populated this region for thousands of years (sandals found near Fort Rock date back 7,000 years).
It’s important to recognize that the descendants of the original inhabitants of this land continue to live and thrive in Central Oregon. Members of the Confederated Tribes of Warm Springs are part of the St. Charles community and are valued caregivers, patients and community members. By acknowledging the past and working towards an inclusive future, St. Charles also aims to be a place where Indigenous professionals can be part of a thriving health care system that uses culturally competent practices for all.
What is the history of the Confederated Tribes of Warm Springs?
The Jefferson County region has long been a place where food was gathered and collected. Tribes used this area as a hub for travel and commerce before settlers came in the 19th Century and well before the Treaty of 1855 was signed with the Mid-Columbia Tribes.
The Confederated Tribes of Warm Springs is comprised of three distinct tribes:
Warm Springs: “Treaty Tribe” This includes many Ichishkiin Speaking tribes historically indigenous to the Jefferson/ Wasco/ Gilliam/ Wheeler/ Crook and Deschutes counties, now spoken of as one group.
Wascos: “Treaty Tribe” Re-located Kiksht Speaking tribes (Cascade Mountains to The Dalles) from the lush Columbia River to the arid High Desert.
Paiutes: “Non-Treaty Tribe” Many Numu Speaking tribes historically indigenous to the area from Deschutes County to western Idaho and south to Tonopah, Nevada and west to Yosemite National Park back to Deschutes County. These tribes were brought to the area after defending their territories against colonization, now a diaspora of people.
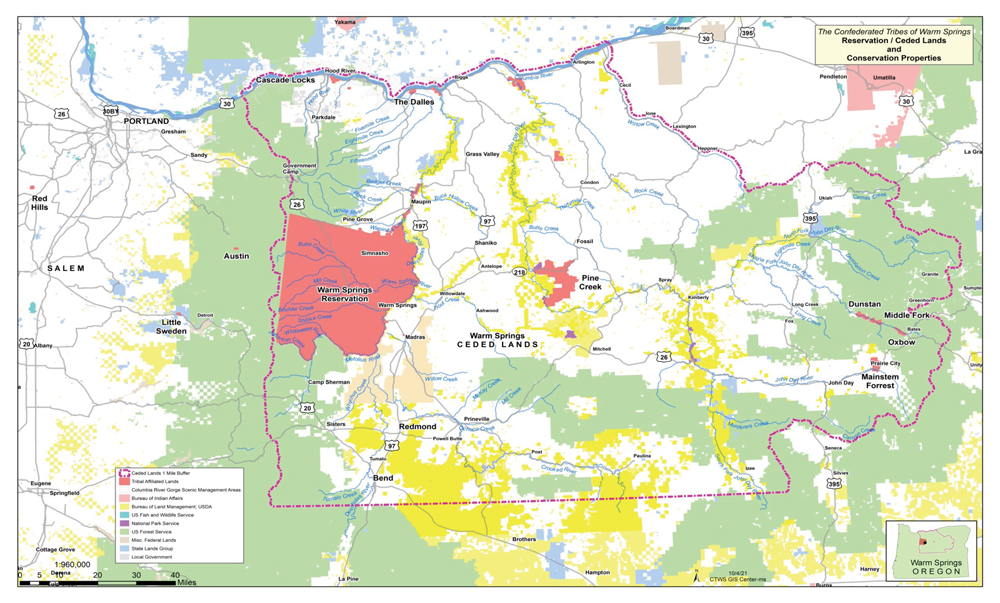
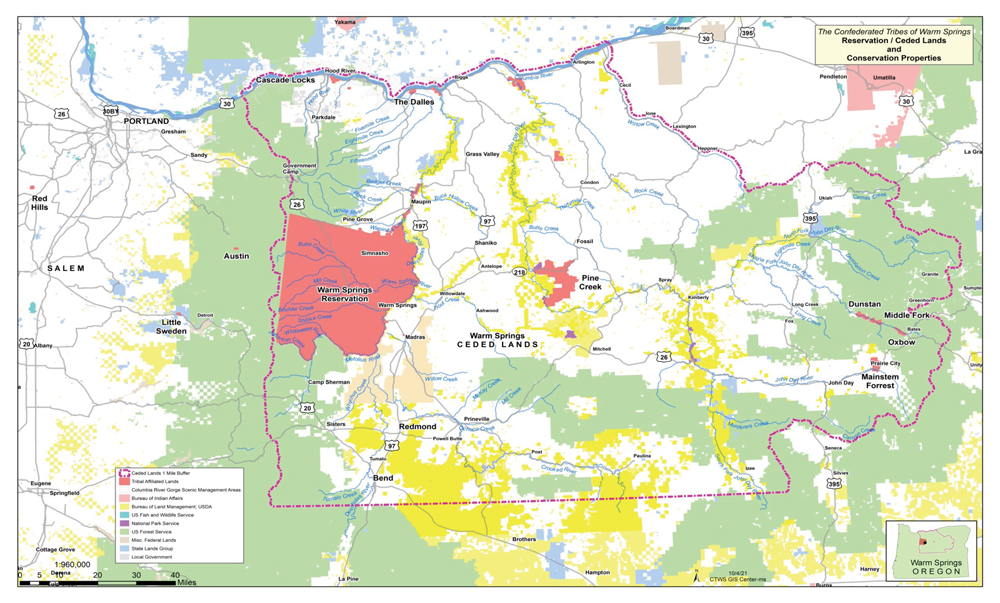
See a map of the land ceded in the treaty with the Middle Bands of Oregon, courtesy of Robert Brunoe, tribal member and Secretary-Treasurer-CEO of the Confederated Tribes of Warm Springs
How was this land acknowledgment created?
St. Charles is grateful to all the partners who helped develop and inspire this project. We give special thanks to the following individuals for offering their insights and support. Thank you to members from the Confederated Tribes of Warm Springs, including Robert Brunoe, Tribal Member and Secretary-Treasurer-CEO of the Confederated Tribes of Warm Springs, and Shilo Shaw Tippett, Ph.D., Tribal Member, clinical psychologist with St. Charles and OHSU assistant professor, for helping create text of the land acknowledgment. Thank you to Rain Circle, Tribal Member, Kiksht language intern with the Cultural and Heritage Department with the Confederated Tribes of Warm Springs, for development and creation of content for the webpage. Thank you to the members of the CEO-appointed task force of St. Charles caregivers appointed to help support this effort, including Vanessa Culps, Tribal Member and a St. Charles caregiver. Thank you also to the many Tribal Members and St. Charles caregivers who provided valuable input, insight and support throughout the process.
Where can the land acknowledgment be found?
Artwork depicting the text of the land acknowledgment can be found in the main entrance of St. Charles Madras. The land acknowledgment is also displayed at all four St. Charles hospitals and several St. Charles clinic locations throughout the region.
What additional actions is St. Charles taking to align with this effort?
St. Charles Health System is committed to partnering with members of the Confederated Tribes of Warm Springs on programs that support increased health, wellness, education, understanding and awareness between our communities.
St. Charles Madras partners with spiritual leaders in Warm Springs to participate in beginning and end of life ceremonies in the hospital setting.
St. Charles was grateful for the opportunity to work closely with community partners in Warm Springs to advocate for passage of new state legislation to allow health care organizations to better support patients’ cultural and spiritual beliefs (the legislation passed in July 2023.) St. Charles is honored to be longtime participants in Native Aspirations, a community group with the focus on health and well-being of the Warm Springs community. Our organization is also honored to participate in the Pi-Ume-Sha health fair held in Warm Springs, one of the largest such fairs in the region. In 2022, St. Charles honored the passing of the Wasco Chief by lowering American flags on the hospital campuses.
Residents who are part of St. Charles' new graduate medical education program (Three Sisters Rural Track Program), will practice medicine at the Indian Health Service Clinic in Warm Springs in addition to serving at St. Charles Madras and other area sites.
St. Charles Madras hosts a quarterly Patient Family Advisory Council meeting with members from local communities, including Warm Springs. We look to members of the council to consistently help us learn and grow in our cultural competencies as a provider of health care in the Central Oregon region and we look forward to continuing to strengthen our relationships into the future.
St. Charles Madras has also hosted a Native Market featuring local vendors from the Confederated Tribes of Warm Springs.
How can individuals learn more about the history, culture and current events related to the Confederated Tribes of Warm Springs and other Indigenous people?
The Tribes host an informative website that includes information on tribal history.
A widespread international campaign is underway to raise awareness about instances of violence against Indigenous people called Missing and Murdered Indigenous Women and Relatives (learn more), and often symbolized by a red hand, often depicted across the mouth of an individual. Learn more by visiting Sovereign Bodies Institute, which has a goal of using “Indigenous traditions data gathering and knowledge transfer to create, disseminate, and put into action research on gender and sexual violence against Indigenous people.”
Oregon State University hosts an in-depth resource for those interested in learning more about land acknowledgments and related resources.
The land acknowledgment in Madras includes many symbols – what do they mean?
The border for the land acknowledgment includes symbols of objects, foods, animals and artifacts of importance to the Confederated Tribes of Warm Springs. Pictured are huckleberries, arrowheads, a root-digging tool, a salmon, a black bear and a basket.